
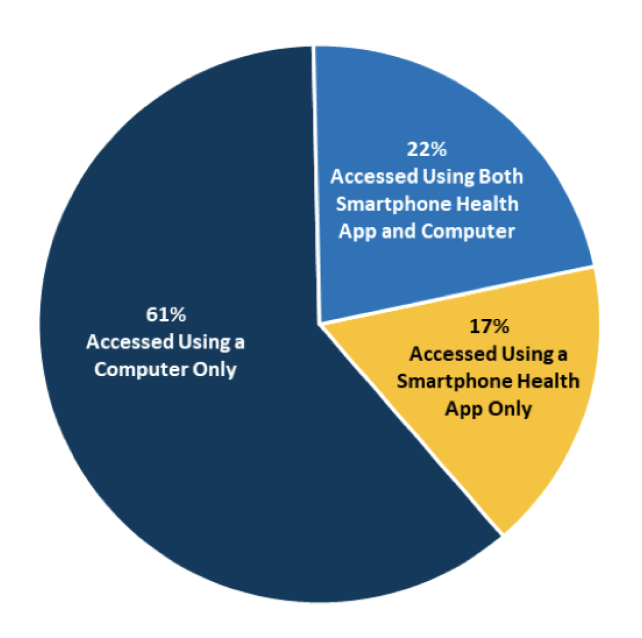
 Source: HINTS 5, Cycle 4 (2020) Notes: Denominator represents individuals who accessed their patient
portal at least once within the past year. Individuals who access their portal at least once in the
past year are referred to as “patient portal users”.
Improved Patient Health Awareness is a key instrument towards improving patient outcomes. The
monitoring capabilities provided by some of the more sophisticated mobile healthcare apps offers
real-time personal health assessments. Patients can then take this information and make more
informed choices. Awareness of any risk factors coupled with educational efforts are shown to
dramatically reduce advanced health complications in patients.
Actualized Data for Providers is equally as important as patient awareness. Physicians can
determine if a course of treatment is appropriate or even effective based upon the data provided by
mobile healthcare apps. 90% of physicians use smartphones to access electronic health records and
information, communicate with peers, or manage their schedule.
Cost Reduction is something that hospital stakeholders are using towards hospital budgeting
efforts – especially following the pandemic. A report, The Digital Revolution Comes to US Healthcare
by Goldman Sachs, cited that virtual health offerings can generate approximately $300 billion in
healthcare savings. Studies also show the biggest cost savings are seen in the avoidance of hospital
readmission and reduced stay times. Clinical trials using mobile technology indicated a 15%-20%
reduction in hospital stays and as much as 30% fewer emergency room visits.
Mobile Healthcare Apps Eases Some of the Challenges
Experienced by Vulnerable Populations
Simply put, vulnerable populations struggle for access to quality healthcare. However, telemedicine
offers a viable alternative to facilitate basic levels of care. With mobile healthcare apps in
place, providers can monitor at-risk patients more effectively. Whether the reasons are because of
transportation issues, language fluency, or a lack of financial resources, mobile healthcare apps
are meeting that need in a virtual sense. On a positive note, there seems to be a willingness to
participate and take part in virtual monitoring efforts by affected patient communities.
“Medical boards and medical associations were hesitant about embracing telehealth; physicians were
concerned about diminishing the relationship they have with patients. But the experiences with
telehealth during the last couple of years have been reassuring, and telehealth increasingly has
become one of the ways physicians interact with patients,” says Roy Schoenberg, CEO of American
Well, one of the leading telehealth companies in the US.
For elderly patients, or those with compromised immune systems, mobile healthcare apps prove to be a
safety conscious solution as well. Ultimately, mobile health app monitoring can give providers an
opportunity to navigate tricky health situations before they have a chance to become more
exaggerated.
Genomic Science and Mobile Health Care Apps
One of the more exciting mobile health developments are those that link DNA findings to mobile
healthcare technologies. DNA testing companies offer genetic health information that ties directly
into managing one's personal health. The genomic information provides a detailed assessment of risk
for certain diseases and recommends tests, nutritional suggestions, and other avenues to bring a
more comprehensive health picture into view. Doctors are readily embracing this type of technology
because it remedies endless troubleshooting, saves diagnostic time and resources, and places every
possible resource in place to better improve patient health and quality of life.
Through the lens of enhanced remote monitoring capabilities (wearables), patient data points can
provide many useful clues relative to diagnosing chronic diseases and conditions. Seemingly minor
details such as sleep habits, allergic reactions, and alcohol consumption can all steer doctors on a
more accurate diagnostic path. Seen as win-win, the medical community welcomes this direction
towards precision-based medicine.
The Future of Mobile Healthcare Applications
Health app developers in many regards are just scratching the surface of what's possible in this
space. Following post-pandemic success and many key takeaways, the mobile healthcare industry is
poised to revolutionize many areas where only a physical doctors visit would satisfy. Research shows
that patients want expanded functionality; meaning they want more than the ability to merely
schedule appointments, reorder prescriptions, and virtually meet with their doctors.
Patient data suggest that many emergencies hospital visits could have been handled with a phone call
or virtual visit. Though this has been met with apprehension on the part of healthcare
administrators, this is a hotbed clinical area where we may see enhanced mobile interaction.
Emergency mobile health care apps such as Quick EM are shown to be very popular in the medical
school arenas. Doctors routinely use their smartphones to reference data and in emergency
situations; this is especially true for interns and practitioners.
Speculations of smartphone enabled apps with capabilities of determining the risk of mole
malignancy, or computerized blood vessel assessments are representative of some of the amazing
developments rumored to be on the horizon. We can also expect increased measures in patient safety
and anti-medical fraud. The use of third-party app partners places a heightened risk of HIPAA
violations, so it makes sense for these vulnerabilities to be addressed in some capacity.
Finding a Balance Between Telehealth and In-Person Patient
Visits
Most in the clinical space fully acknowledge, mobile health care are not a one size fits all
dynamic. Seemingly even mobile app developers recognize a great need for user adaptation and growth
in this space. App user data indicates most of the healthcare apps have less than 10,000 downloads.
There are more than 400,000 healthcare apps available in the app stores, but very few of them have
succeeded. This statistic translates to the fact that a balance is still being negotiated by
consumers and providers alike.
While the pandemic may have given consumers a reason to gravitate to learn more about what’s
available, the user paradigm shift isn’t necessarily a given. Mobile app developers will have to
work hard to find out exactly what will drive more patients to use their apps and then in turn make
sure the app can fulfill that need. The big exclamation point is that mobile healthcare apps have
the potential to saving lives and that is deserving of whatever efforts are made in this
ever-evolving space.
https://medium.com/geekculture/mobile-healthcare-apps-in-2022-top-benefits-challenges-eac0f415e269
EXPERT REVIEW OF MEDICAL DEVICES, 2016VOL.
13, NO. 9, 823–830http://dx.doi.org/10.1080/17434440.2016.1218277© 2016 The Author(s). Published
by Informa UK Limited, trading as Taylor & Francis GroupThis is an Open Access article
distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives
License (http://creativecommons.org/licenses/by-nc-nd/4.0/),which permits non-commercial re-use,
distribution, and reproduction in any medium, provided the original work is properly cited, and
is not altered, transformed, or built upon in any way
https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.120.007031
Inbal Nahum-Shani, PhD, Shawna N Smith, PhD,
Bonnie J Spring, PhD, Linda M Collins, PhD, Katie Witkiewitz, PhD, Ambuj Tewari, PhD, Susan A
Murphy, PhD, Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and
Design Principles for Ongoing Health Behavior Support, Annals of Behavioral Medicine, Volume 52,
Issue 6, June 2018, Pages 446–462, https://doi.org/10.1007/s12160-016-9830-8
Source: HINTS 5, Cycle 4 (2020) Notes: Denominator represents individuals who accessed their patient
portal at least once within the past year. Individuals who access their portal at least once in the
past year are referred to as “patient portal users”.
Improved Patient Health Awareness is a key instrument towards improving patient outcomes. The
monitoring capabilities provided by some of the more sophisticated mobile healthcare apps offers
real-time personal health assessments. Patients can then take this information and make more
informed choices. Awareness of any risk factors coupled with educational efforts are shown to
dramatically reduce advanced health complications in patients.
Actualized Data for Providers is equally as important as patient awareness. Physicians can
determine if a course of treatment is appropriate or even effective based upon the data provided by
mobile healthcare apps. 90% of physicians use smartphones to access electronic health records and
information, communicate with peers, or manage their schedule.
Cost Reduction is something that hospital stakeholders are using towards hospital budgeting
efforts – especially following the pandemic. A report, The Digital Revolution Comes to US Healthcare
by Goldman Sachs, cited that virtual health offerings can generate approximately $300 billion in
healthcare savings. Studies also show the biggest cost savings are seen in the avoidance of hospital
readmission and reduced stay times. Clinical trials using mobile technology indicated a 15%-20%
reduction in hospital stays and as much as 30% fewer emergency room visits.
Mobile Healthcare Apps Eases Some of the Challenges
Experienced by Vulnerable Populations
Simply put, vulnerable populations struggle for access to quality healthcare. However, telemedicine
offers a viable alternative to facilitate basic levels of care. With mobile healthcare apps in
place, providers can monitor at-risk patients more effectively. Whether the reasons are because of
transportation issues, language fluency, or a lack of financial resources, mobile healthcare apps
are meeting that need in a virtual sense. On a positive note, there seems to be a willingness to
participate and take part in virtual monitoring efforts by affected patient communities.
“Medical boards and medical associations were hesitant about embracing telehealth; physicians were
concerned about diminishing the relationship they have with patients. But the experiences with
telehealth during the last couple of years have been reassuring, and telehealth increasingly has
become one of the ways physicians interact with patients,” says Roy Schoenberg, CEO of American
Well, one of the leading telehealth companies in the US.
For elderly patients, or those with compromised immune systems, mobile healthcare apps prove to be a
safety conscious solution as well. Ultimately, mobile health app monitoring can give providers an
opportunity to navigate tricky health situations before they have a chance to become more
exaggerated.
Genomic Science and Mobile Health Care Apps
One of the more exciting mobile health developments are those that link DNA findings to mobile
healthcare technologies. DNA testing companies offer genetic health information that ties directly
into managing one's personal health. The genomic information provides a detailed assessment of risk
for certain diseases and recommends tests, nutritional suggestions, and other avenues to bring a
more comprehensive health picture into view. Doctors are readily embracing this type of technology
because it remedies endless troubleshooting, saves diagnostic time and resources, and places every
possible resource in place to better improve patient health and quality of life.
Through the lens of enhanced remote monitoring capabilities (wearables), patient data points can
provide many useful clues relative to diagnosing chronic diseases and conditions. Seemingly minor
details such as sleep habits, allergic reactions, and alcohol consumption can all steer doctors on a
more accurate diagnostic path. Seen as win-win, the medical community welcomes this direction
towards precision-based medicine.
The Future of Mobile Healthcare Applications
Health app developers in many regards are just scratching the surface of what's possible in this
space. Following post-pandemic success and many key takeaways, the mobile healthcare industry is
poised to revolutionize many areas where only a physical doctors visit would satisfy. Research shows
that patients want expanded functionality; meaning they want more than the ability to merely
schedule appointments, reorder prescriptions, and virtually meet with their doctors.
Patient data suggest that many emergencies hospital visits could have been handled with a phone call
or virtual visit. Though this has been met with apprehension on the part of healthcare
administrators, this is a hotbed clinical area where we may see enhanced mobile interaction.
Emergency mobile health care apps such as Quick EM are shown to be very popular in the medical
school arenas. Doctors routinely use their smartphones to reference data and in emergency
situations; this is especially true for interns and practitioners.
Speculations of smartphone enabled apps with capabilities of determining the risk of mole
malignancy, or computerized blood vessel assessments are representative of some of the amazing
developments rumored to be on the horizon. We can also expect increased measures in patient safety
and anti-medical fraud. The use of third-party app partners places a heightened risk of HIPAA
violations, so it makes sense for these vulnerabilities to be addressed in some capacity.
Finding a Balance Between Telehealth and In-Person Patient
Visits
Most in the clinical space fully acknowledge, mobile health care are not a one size fits all
dynamic. Seemingly even mobile app developers recognize a great need for user adaptation and growth
in this space. App user data indicates most of the healthcare apps have less than 10,000 downloads.
There are more than 400,000 healthcare apps available in the app stores, but very few of them have
succeeded. This statistic translates to the fact that a balance is still being negotiated by
consumers and providers alike.
While the pandemic may have given consumers a reason to gravitate to learn more about what’s
available, the user paradigm shift isn’t necessarily a given. Mobile app developers will have to
work hard to find out exactly what will drive more patients to use their apps and then in turn make
sure the app can fulfill that need. The big exclamation point is that mobile healthcare apps have
the potential to saving lives and that is deserving of whatever efforts are made in this
ever-evolving space.
https://medium.com/geekculture/mobile-healthcare-apps-in-2022-top-benefits-challenges-eac0f415e269
EXPERT REVIEW OF MEDICAL DEVICES, 2016VOL.
13, NO. 9, 823–830http://dx.doi.org/10.1080/17434440.2016.1218277© 2016 The Author(s). Published
by Informa UK Limited, trading as Taylor & Francis GroupThis is an Open Access article
distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives
License (http://creativecommons.org/licenses/by-nc-nd/4.0/),which permits non-commercial re-use,
distribution, and reproduction in any medium, provided the original work is properly cited, and
is not altered, transformed, or built upon in any way
https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.120.007031
Inbal Nahum-Shani, PhD, Shawna N Smith, PhD,
Bonnie J Spring, PhD, Linda M Collins, PhD, Katie Witkiewitz, PhD, Ambuj Tewari, PhD, Susan A
Murphy, PhD, Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and
Design Principles for Ongoing Health Behavior Support, Annals of Behavioral Medicine, Volume 52,
Issue 6, June 2018, Pages 446–462, https://doi.org/10.1007/s12160-016-9830-8
| LETS WORK TOGETHER Contact Us For a Free Consultation |